KeyHealth Medical Aid Scheme
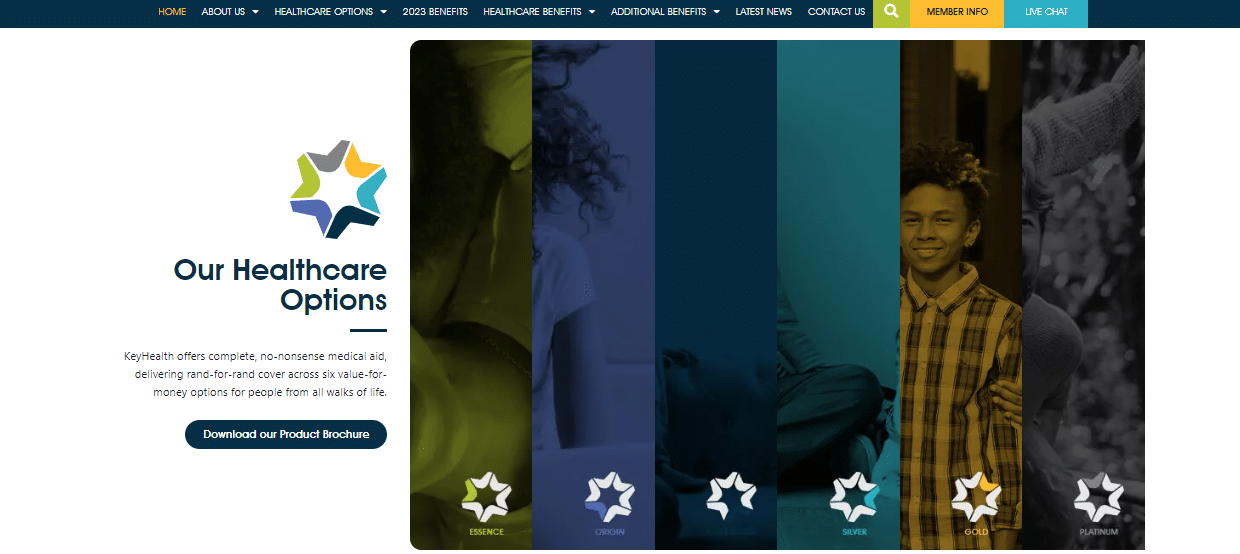
Overall, KeyHealth offers 6 medical aid plans (Essence, Origin, Equilibrium, Silver, Gold, and Platinum Option) starting from R1990 per month. Additionally, KeyHealth offers 24/7 support and offers a comprehensive gap cover on every policy.
| 🔎 Medical Aid | 🥇 KeyHealth |
| 📌 Registration Number | 1087/CMS |
| 👥 The average number of members | 150,000+ |
| 📍 Number of Markets | South Africa |
| 👤 Number of Employees | 500+ |
| 📈 Market Share | |
| 📉 Listed on the JSE | ❎ No |
| 📊 JSE Stock Symbol | None |
| ➡️ The most recent Market Cap reported | None |
| ❤️ Average Customer Rating | 3/5 |
KeyHealth Review – Analysis of Medical Aids’ Main Features
- ✅ KeyHealth at a Glance
- ✅ KeyHealth Regulation
- ✅ KeyHealth Plan Overview
- ✅ KeyHealth – Advantages over Competitors
- ✅ KeyHealth Medical Savings Account
- ✅ How to apply for Medical Aid with KeyHealth
- ✅ How to Submit a Claim with KeyHealth
- ✅ How to Submit a Compliment or Complaint with KeyHealth
- ✅ How to Switch my Medical Aid to KeyHealth
- ✅ KeyHealth vs Discovery Health vs Bonitas – A Comparison
- ✅ KeyHealth Member Reviews
- ✅ KeyHealth – Our Verdict
- ✅ KeyHealth Pros and Cons
- ✅ KeyHealth Frequently Asked Questions
Medical Aid KeyHealth at a Glance
| 🔎 Medical Aid | 🥇 KeyHealth |
| ➡️ Headquartered | Gauteng, South Africa |
| 📎 Registration Number | 1087/CMS |
| 👥 The average number of members | 150,000+ |
| 📌 Number of Markets | South Africa |
| 👤 Number of Employees | 500+ |
| 📈 Listed on the JSE | No |
| 📉 JSE Stock Symbol | None |
| 📊 The most recent Market Cap reported | None |
| ❤️ Average Customer Rating | 3/5 |
| ✔️ Average Number of Reviews | 200+ |
| 🚩 Market Share | |
| 6️⃣ Number of plans | 6 |
| 🚑 Number of Hospitals in Network | 184+ |
| 🏠 Home care provided | No |
| ⚠️ Sponsorships | None |
| 📱 Mobile App | Yes, iOS and Android |
| 📖 KeyHealth Magazine for clients | No |
| 💻 Medical Claims Portal | ✅ Yes |
| 🖥️ Information Hub for COVID-19 | None |
| ⚕️ Chronic Illness Benefits | ✅ Yes |
| 📌 Number of PMB Diagnoses | 26 |
| ➡️ Screening and Prevention offered | ✅ Yes |
| 👶 Maternity Benefit | ✅ Yes |
| 💵 Medical Aid Contribution Range (ZAR) | 1,990 – 11,308 ZAR |
| ⛔ Average Waiting Period | Three to twelve months |
| 💴 Late-joiner penalties charged | ✅ Yes |
| 🌎 Is International Medical Cover offered | ✅ Yes |
| 💷 International Travel Benefit (ZAR) | From 2.5 to 6 million ZAR per beneficiary |

KeyHealth Regulation
The Council for Medical Schemes regulates KeyHealth Medical Scheme. The Council governs South Africa’s medical plan business for Medical Schemes (CMS), a regulating body set up under the Medical Schemes Act, No. 131 of 1998 (the Act). The CMS is responsible for a range of tasks related to the oversight of medical insurance plans, such as:
- Responsible for registering medical insurance plans and ensuring they comply with the law and other laws.
- Making sure healthcare plans have the money to pay claims.
- Examining and authorizing proposed price hikes for medical plans.
- Accepting and examining member complaints and initiating disciplinary action against medical plans that violate the Act or other applicable rules.
- Helping medical insurance plans follow the law and other laws.
Furthermore, if a medical scheme is found to violate the law, the CMS has the authority to issue administrative fines and penalties.
KeyHealth Plan Overview
| 🔎 Plan | 💴 Contributions (Main) | 💵 Contributions (+ Adult) | 💶 Contributions (+ Child) | 💷 Medical Savings (Up to) | 💳 Day-to-Day Cover Benefit Value (annually) | 🚑 Hospital Benefit Value | ⚕️ Chronic Conditions |
| 1️⃣ Essence | 1,990 ZAR | 1,595 ZAR | 717 ZAR | None | None | Unlimited |
· 1,830 ZAR (+1 Adult)
· 1,500 ZAR (+1 Adult)
· 2,380 ZAR (+1 Adult)
· 6,760 ZAR (+1 Adult)
· 5,700 ZAR (+1 Adult)
· 4,480 ZAR (+1 Adult)
· 12,675 ZAR (+1 Adult)
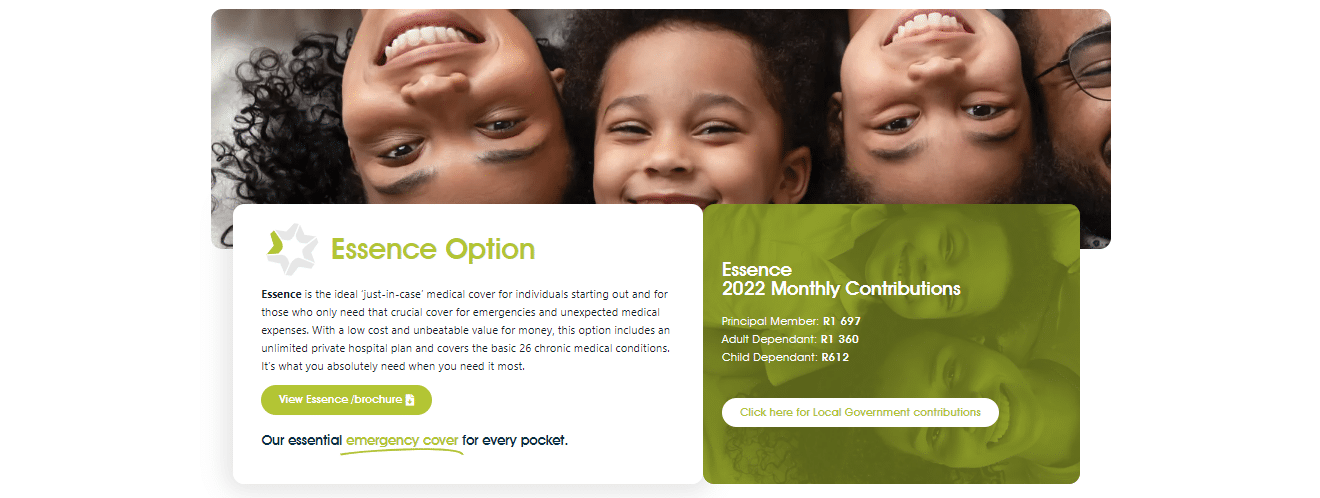
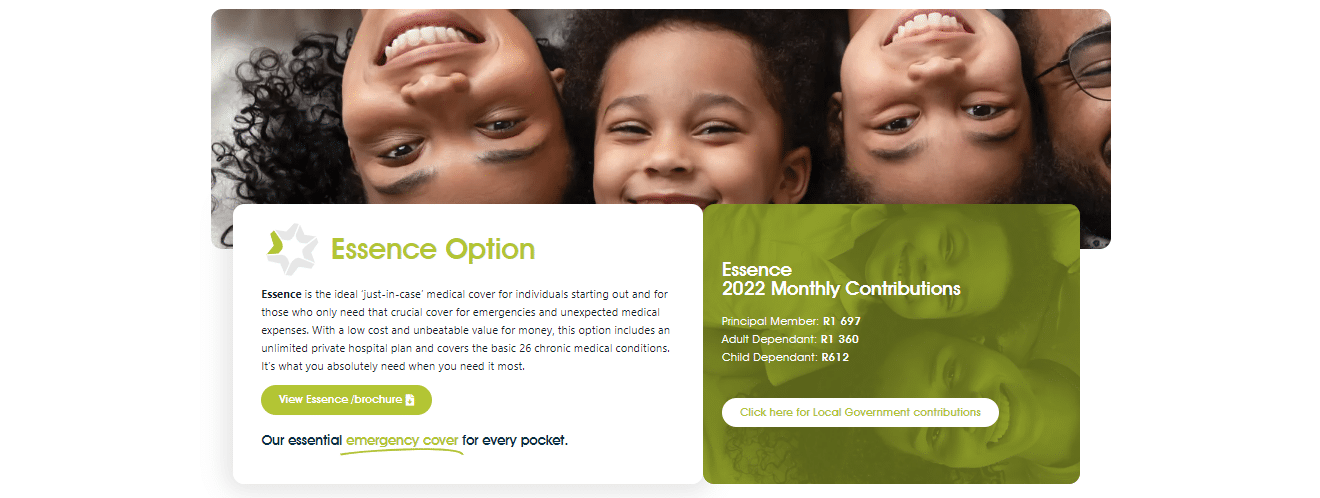
Essence
Essence is the best “just-in-case” medical cover for young individuals just starting their careers and those who require cover simply for emergencies and unanticipated medical bills. The Essence package includes unlimited private hospital coverage and covers the 26 most common chronic medical diseases at an amazing price.
Hospital Expenses
- All treatment-related expenses at Life Healthcare and Netcare hospitals nationwide, Mediclinic hospitals in the Western Cape, Bloemfontein, Polokwane, and other chosen hospitals (DSP hospital network) will be covered in full.
- Furthermore, there is no limit to the number of hospital admissions. However, all in-hospital operations must be pre-authorized before admission.
- Members get unlimited coverage in-hospital. However, a 30% co-payment will be applied to the hospital bill if a non-DSP hospital is utilized voluntarily.
Injuries resulting from accidents
- Unlimited cover.
- Most incidents are considered PMBs (Prescribed Minimum Benefits), and the scheme will cover the treatment of such injuries, including hospitalization, in full by the Scheme according to its regulations and clinical guidelines.
In-Hospital Specialist Services
- The Scheme covers services rendered by any Specialist while the member is hospitalized.
Oncology
- The diagnosis and treatment of problems associated with cancer.
- The benefit value is up to 180,000 ZAR per family per year.
Scans
- Includes diagnostic scans performed both in and out of the hospital.
- The value of the benefit is 19,000 ZAR per family per year.
Chronic Medication
- KeyHealth gives unlimited coverage on medication and is used constantly for at least three months to treat one of the 26 CDL (Chronic Disease List) diseases.
Supplementary Services
- Psychiatric Treatment is an in-hospital benefit that requires pre-authorization. The benefit is 22,900 ZAR per family per year, and case management will apply. Furthermore, for treatment Out-of-Hospital, PMB entitlement applies.
- Prosthesis / Prosthetics – PBM entitlement and Pre-authorization is compulsory. Furthermore, treatment is subject to the following:
- Emergency transport by ambulance – Netcare 911 (provider of DSP) provides members with emergency transport by road or air ambulance from the scene of an accident, as well as medically justifiable inter-hospital transfers.
- Medical Appliances – The provision of medical equipment, such as wheelchairs, crutches, and contraceptive devices, for treating and curing medical disorders or processes. This benefit is 8,400 ZAR per family and year.
- Endoscopic procedures / Scopes – All scopes are fully covered if performed in a DSP hospital.
Prescribed Minimum Benefits (PMB)
Prescribed Certain Benefits (PMBs) are a set of statutorily defined benefits designed to ensure that all medical plan members are entitled to a minimum level of health care, regardless of the benefit option they have selected.
Additional Benefits
- Easy-ER – Easy-ER is a first-of-its-kind KeyHealth project that provides all KeyHealth members with immediate access to the emergency room (ER) of a hospital for emergency medical care.
- Smart Baby – The Smart Baby Program from KeyHealth provides excellent maternity benefits, support, and general wellness counseling for the pregnant mother.
Excluded items on Essence:
- Prosthesis Benefits
- Specialized Dentistry
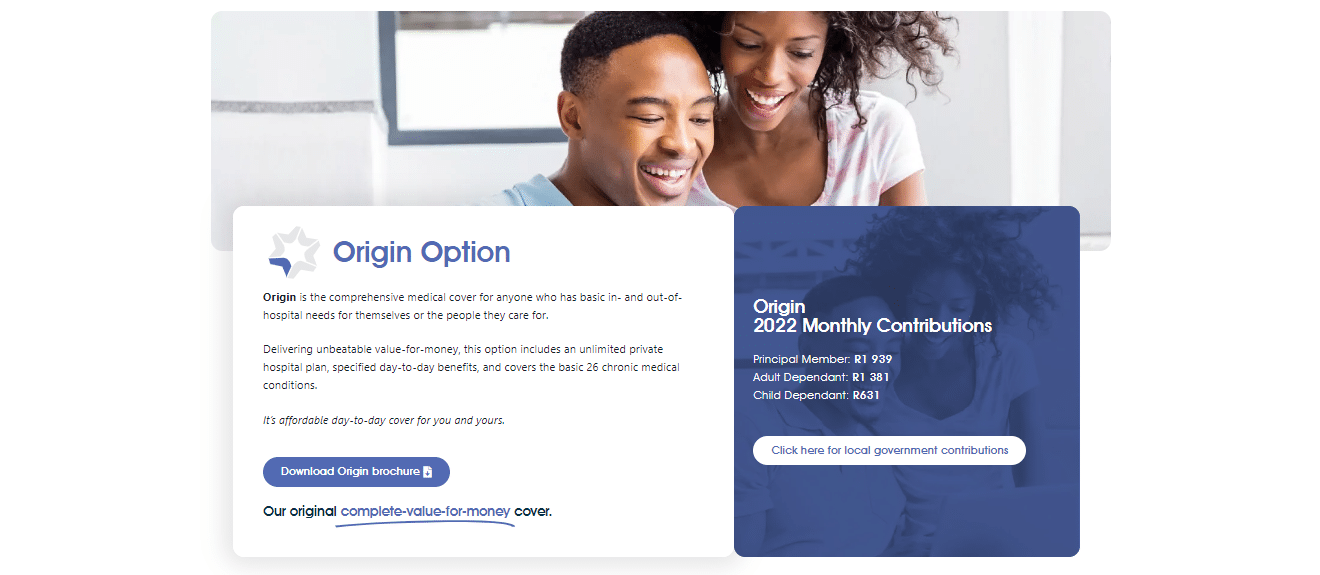
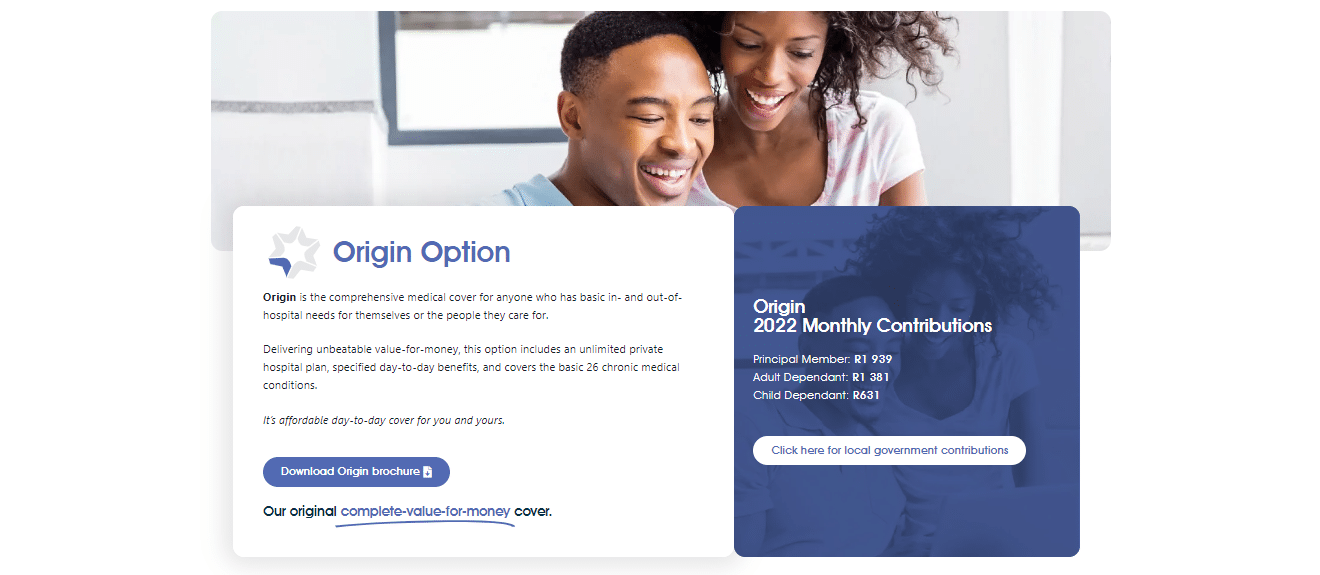
Origin
Origin is the comprehensive medical cover for everyone with basic in-hospital and out-of-hospital medical needs for themselves or their dependents. The Origin plan contains an unlimited private hospital plan and specified day-to-day benefits. In addition, the Origin plan covers the 26 most prevalent chronic medical problems.
Hospital Expenses
- All treatment-related expenses at Life Healthcare and Netcare hospitals nationwide, Mediclinic hospitals in the Western Cape, Bloemfontein, Polokwane, and other chosen hospitals (DSP hospital network) will be covered in full.
- Furthermore, there is no limit to the number of hospital admissions. However, all in-hospital operations must be pre-authorized before admission.
- Members get unlimited coverage in-hospital. However, a 30% co-payment will be applied to the hospital bill if a non-DSP hospital is utilized voluntarily.
Injuries resulting from accidents
- Unlimited cover.
- Most incidents are considered PMBs (Prescribed Minimum Benefits), and the scheme will cover the treatment of such injuries, including hospitalization, in full by the Scheme according to its regulations and clinical guidelines.
In-Hospital Specialist Services
- The Scheme covers services rendered by any Specialist while the member is hospitalized.
Oncology
- The diagnosis and treatment of problems associated with cancer.
- The benefit value is up to 180,000 ZAR per family per year.
Scans
- Includes diagnostic scans performed both in and out of the hospital.
- The value of the benefit is 19,000 ZAR per family per year.
Day-to-Day Medical Expenses
- Routine Medical Expenses – Includes general practitioner and specialist consultations, X-rays, prescribed (acute) and over-the-counter drugs, blood tests, physiotherapy, optical, dentistry, etc.
Dentistry
- This KeyHealth plan provides conservative dental care to members, including dentist consultation, x-rays, oral hygiene care, fillings, and extractions.
- Benefit value is contingent on the amount available for standard benefit allocation.
Chronic Medication
- There is unlimited coverage on the medication used constantly for at least three months to treat one of the 26 CDL (Chronic Disease List) diseases.
Supplementary Services
- Psychiatric Treatment is an in-hospital benefit that requires pre-authorization. The benefit is 22,900 ZAR per family per year, and case management will apply. Furthermore, for treatment Out-of-Hospital, PMB entitlement applies.
- Prosthesis / Prosthetics – PBM entitlement and Pre-authorization is compulsory.
- Emergency transport by ambulance – Netcare 911 (provider of DSP) provides members with emergency transport by road or air ambulance from the scene of an accident, as well as medically justifiable inter-hospital transfers.
- Medical Appliances – The provision of medical equipment, such as wheelchairs, crutches, and contraceptive devices, for treating and curing medical disorders or processes. This benefit is 8,400 ZAR per family and year.
- Endoscopic procedures / Scopes – All scopes are fully covered if performed in a DSP hospital.
Prescribed Minimum Benefits (PMB)
Prescribed Certain Benefits (PMBs) are a set of statutorily defined benefits designed to ensure that all medical plan members are entitled to a minimum level of health care, regardless of the benefit option they have selected.
Additional Benefits
- Easy-ER – Easy-ER is a first-of-its-kind KeyHealth project that provides all KeyHealth members with immediate access to the emergency room (ER) of a hospital for emergency medical care.
- Health Booster – Preventative health care and diagnostic screenings are provided to Scheme participants at no additional cost. However, the Essence option is excluded from this benefit.
- Smart Baby – The Smart Baby Program from KeyHealth provides excellent maternity benefits, support, and general wellness counseling for the pregnant mother.
Excluded items on Origin:
- Prosthesis Benefits
- Specialized Dentistry
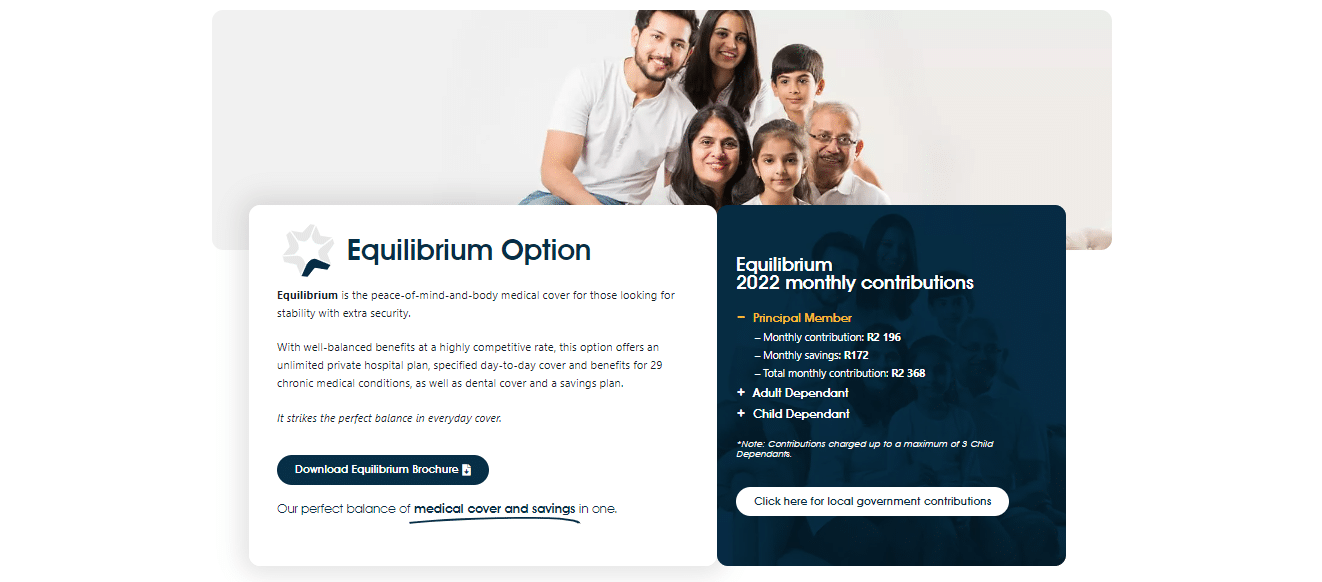
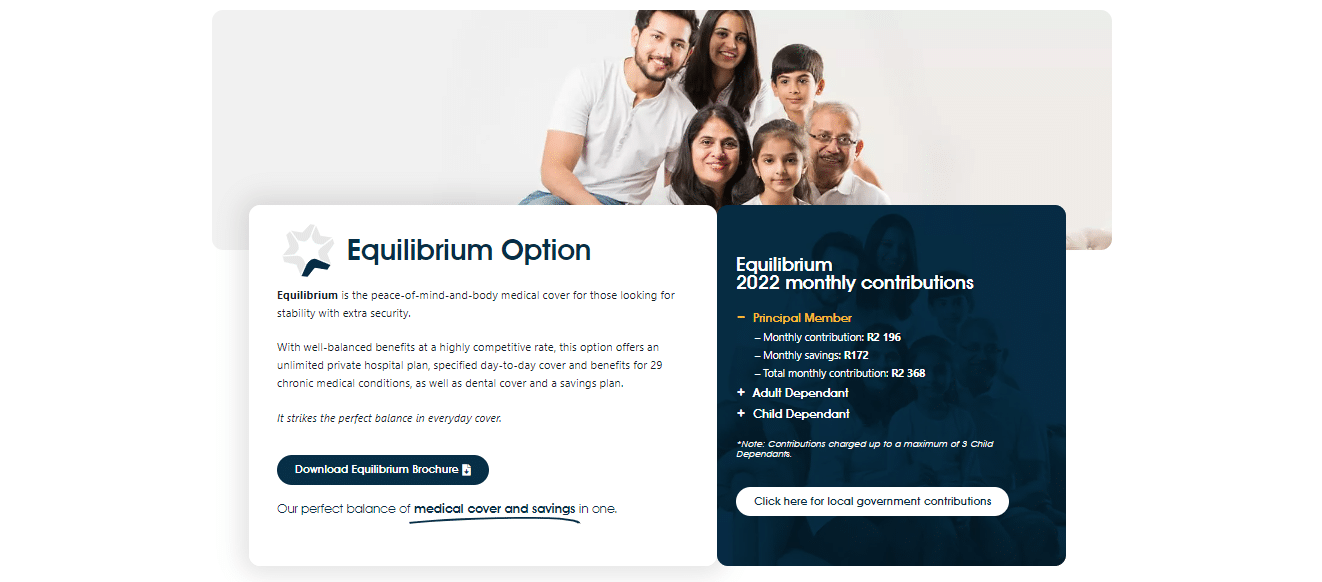
Equilibrium
Equilibrium is the peace-of-mind-and-body medical insurance for individuals seeking stability with added protection. Additionally, KeyHealth Medical Aid’s Equilibrium option presents a comprehensive package that includes unrestricted private hospital coverage, specified daily benefits, and coverage for 29 chronic medical conditions, as well as dental care and a savings plan.
Hospital Expenses
- All treatment-related expenses at Life Healthcare and Netcare hospitals nationwide, Mediclinic hospitals in the Western Cape, Bloemfontein, Polokwane, and other chosen hospitals (DSP hospital network) will be covered in full.
- Furthermore, there is no limit to the number of hospital admissions. However, all in-hospital operations must be pre-authorized before admission.
- Members get unlimited coverage in-hospital. However, a 30% co-payment will be applied to the hospital bill if a non-DSP hospital is utilized voluntarily.
Injuries resulting from accidents
- Unlimited cover.
- Most incidents are considered PMBs (Prescribed Minimum Benefits), and the scheme will cover the treatment of such injuries, including hospitalization, in full by the Scheme according to its regulations and clinical guidelines.
In-Hospital Specialist Services
- The Scheme covers services rendered by any Specialist while the member is hospitalized.
Oncology
- The diagnosis and treatment of problems associated with cancer.
- The benefit value is up to 180,000 ZAR per family per year.
Scans
- Includes diagnostic scans performed both in and out of the hospital.
- The Benefit value of scans is R20,000 per family each year for both in-hospital and out-of-hospital benefits. Co-payment of R1 500 for each scan, in or out of the hospital (except for confirmed PMBs).
Day-to-Day Medical Expenses
- At the start of the year, a portion of a member’s monthly payment is assigned in advance to an MSA, which is used to cover day-to-day medical expenses. The MSA can also be used to pay for expenses not covered by the Scheme and is carried forward to the next year if there is a positive balance at the end of that year. Because this is a family benefit, only one family member can use the entire benefit allocation.
Dentistry
- This plan provides conservative dental care to members, including dentist consultation, x-rays, oral hygiene care, fillings, and extractions.
- Specialized Dental Treatment – Orthodontics (non-cosmetic therapy only). Furthermore, each calendar year, one beneficiary per family can begin therapy. In addition, beneficiaries eligible for treatment are between the ages of 9 and 18.
- The Benefit Value is 80%, subject to scheme conditions.
Chronic Medication
- There is unlimited coverage on the medication used constantly for at least three months to treat one of the 26 CDL (Chronic Disease List) diseases.
- Additional Chronic Medication – Prescribed medication is taken continuously for 3 months or more for three additional chronic diseases and is not on the CDL (Chronic Disease List) for children under the age of 21.
Supplementary Services
- Psychiatric Treatment is an in-hospital benefit that requires pre-authorization. The benefit is 22,900 ZAR per family per year, and case management will apply. Furthermore, for treatment Out-of-Hospital, PMB entitlement applies.
- Prosthesis / Prosthetics – 3,750 ZAR is dedicated per family year, a combined benefit. Pre-authorization is compulsory.
- Emergency transport by ambulance – Netcare 911 (provider of DSP) provides members with emergency transport by road or air ambulance from the scene of an accident, as well as medically justifiable inter-hospital transfers.
- Medical Appliances – The provision of medical equipment, such as wheelchairs, crutches, and contraceptive devices, for treating and curing medical disorders or processes. This benefit is 8,400 ZAR per family and year.
- Endoscopic procedures / Scopes – All scopes are fully covered if performed in a DSP hospital.
Prescribed Minimum Benefits (PMB)
Prescribed Certain Benefits (PMBs) are a set of statutorily defined benefits designed to ensure that all medical plan members are entitled to a minimum level of health care, regardless of the benefit option they have selected.
Additional Benefits
- Easy-ER – Easy-ER is a first-of-its-kind KeyHealth project that provides all KeyHealth members with immediate access to the emergency room (ER) of a hospital for emergency medical care.
- Health Booster – Preventative health care and diagnostic screenings are provided to Scheme participants at no additional cost. However, the Essence option is excluded from this benefit.
- Smart Baby – The Smart Baby Program from KeyHealth provides excellent maternity benefits, support, and general wellness counseling for the pregnant mother.
Excluded items on Equilibrium:
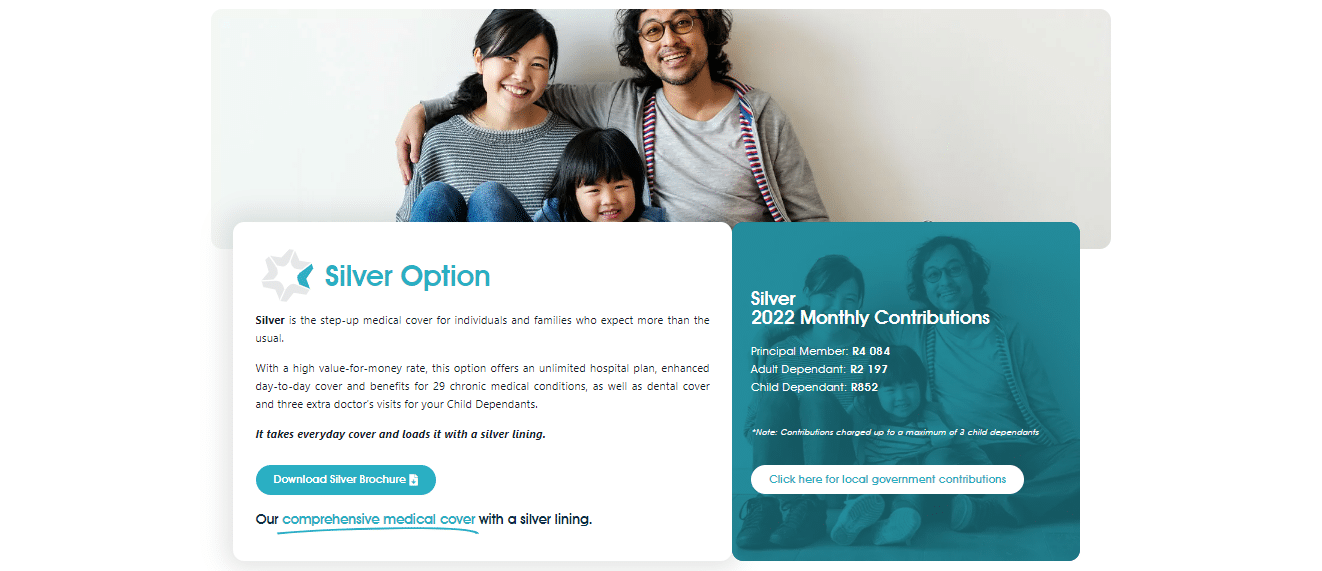
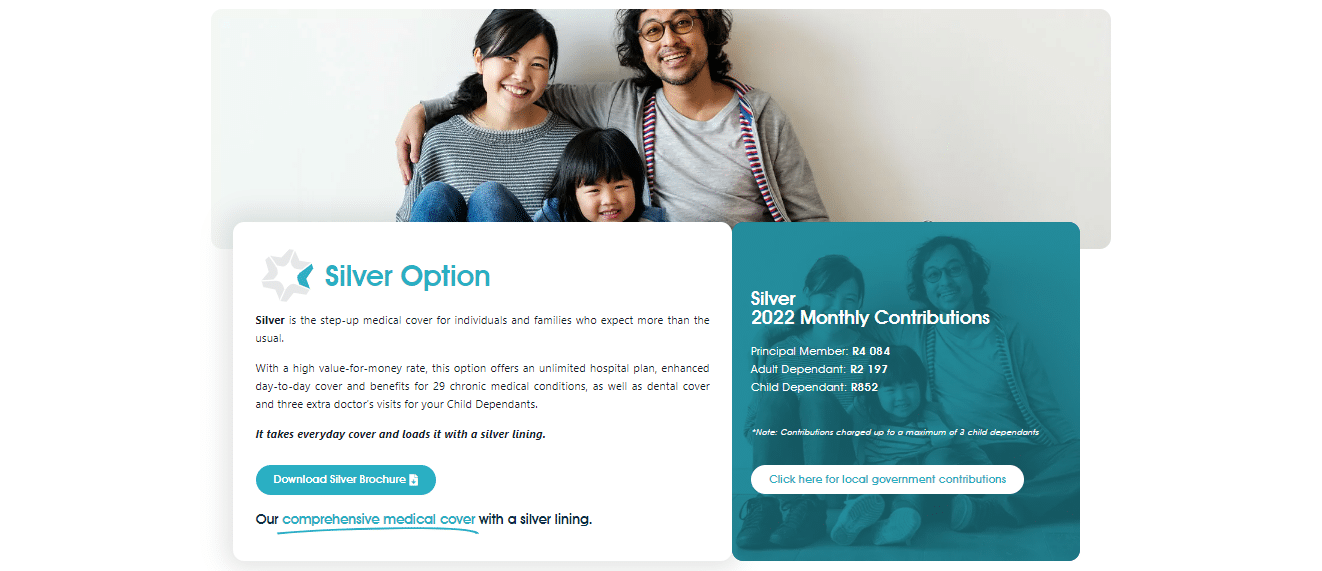
Silver
Individuals and families who expect more than the standard medical coverage are eligible for Silver coverage. The Silver Option offers an unlimited hospital plan, expanded day-to-day cover and benefits for 29 chronic medical conditions, dental cover, and three additional doctor’s appointments for your Child’s Dependents at a price that represents excellent value.
Hospital Expenses
- All treatment-related expenses at Life Healthcare and Netcare hospitals nationwide, Mediclinic hospitals in the Western Cape, Bloemfontein, Polokwane, and other chosen hospitals (DSP hospital network) will be covered in full.
- Furthermore, there is no limit to the number of hospital admissions. However, all in-hospital operations must be pre-authorized before admission.
- Members get unlimited coverage in-hospital. However, a 30% co-payment will be applied to the hospital bill if a non-DSP hospital is utilized voluntarily.
Injuries resulting from accidents
- Unlimited cover.
- Most incidents are considered PMBs (Prescribed Minimum Benefits), and the scheme will cover the treatment of such injuries, including hospitalization, in full by the Scheme according to its regulations and clinical guidelines.
In-Hospital Specialist Services
- The Scheme covers services rendered by any Specialist while the member is hospitalized.
Oncology
- The diagnosis and treatment of problems associated with cancer.
- The benefit value is up to 202,000 ZAR per family per year.
Scans
- Includes diagnostic scans performed both in and out of the hospital.
- Benefits value: R20,000 per family annually for both in-hospital and out-of-hospital benefits. Co-payment of R1 500 for each scan, in or out of the hospital (except for confirmed PMBs).
Sub-acute Facilities and Wound Care
- Covers both in-hospital and out-of-hospital services delivered following an operation or procedure at a rehabilitation or step-down facility and private nursing care to aid in the patient’s recovery.
- Care for wounds is included in this benefit. The Benefit Value is R34 200 and includes wound care up to an annual maximum of R10,950 per family. Combined in-hospital and out-of-hospital coverage.
Day-to-Day Medical Expenses
- Routine Medical Expenses – Includes general practitioner and specialist consultations, X-rays, prescribed (acute) and over-the-counter drugs, blood tests, physiotherapy, optical, dentistry, etc.
Dentistry
- This plan provides conservative dental care to members, including dentist consultation, x-rays, oral hygiene care, fillings, and extractions.
- Specialized Dental Treatment – Orthodontics (non-cosmetic therapy only). Furthermore, each calendar year, one beneficiary per family can begin therapy. In addition, beneficiaries eligible for treatment are between the ages of 9 and 18.
- The Benefit Value is 80%, subject to scheme conditions.
Chronic Medication
- There is unlimited coverage on the medication used constantly for at least three months to treat one of the 26 CDL (Chronic Disease List) diseases.
- Additional Chronic Medication – Prescribed medication is taken continuously for 3 months or more for three additional chronic diseases, not on the CDL (Chronic Disease List) for children under the age of 21.
Supplementary Services
- Psychiatric Treatment is an in-hospital benefit that requires pre-authorization. The benefit is 22,900 ZAR per family per year, and case management will apply. Furthermore, for treatment Out-of-Hospital, PMB entitlement applies.
- Prosthesis / Prosthetics / Fixation Devices – 7,300 ZAR is dedicated per family year, a combined benefit. Pre-authorization is compulsory.
- Emergency transport by ambulance – Netcare 911 (provider of DSP) provides members with emergency transport by road or air ambulance from the scene of an accident, as well as medically justifiable inter-hospital transfers.
- Medical Appliances – The provision of medical equipment, such as wheelchairs, crutches, and contraceptive devices, for treating and curing medical disorders or processes. This benefit is 8,700 ZAR per family and year.
- Endoscopic procedures / Scopes – All scopes are fully covered if performed in a DSP hospital.
Prescribed Minimum Benefits (PMB)
Prescribed Certain Benefits (PMBs) are a set of statutorily defined benefits designed to ensure that all medical plan members are entitled to a minimum level of health care, regardless of the benefit option they have selected.
Additional Benefits
- Easy-ER – Easy-ER is a first-of-its-kind KeyHealth project that provides all KeyHealth members with immediate access to the emergency room (ER) of a hospital for emergency medical care.
- Health Booster – Preventative health care and diagnostic screenings are provided to Scheme participants at no additional cost. However, the Essence option is excluded from this benefit.
- Smart Baby – The Smart Baby Program from KeyHealth provides excellent maternity benefits, support, and general wellness counseling for the pregnant mother.
Excluded items on Silver:
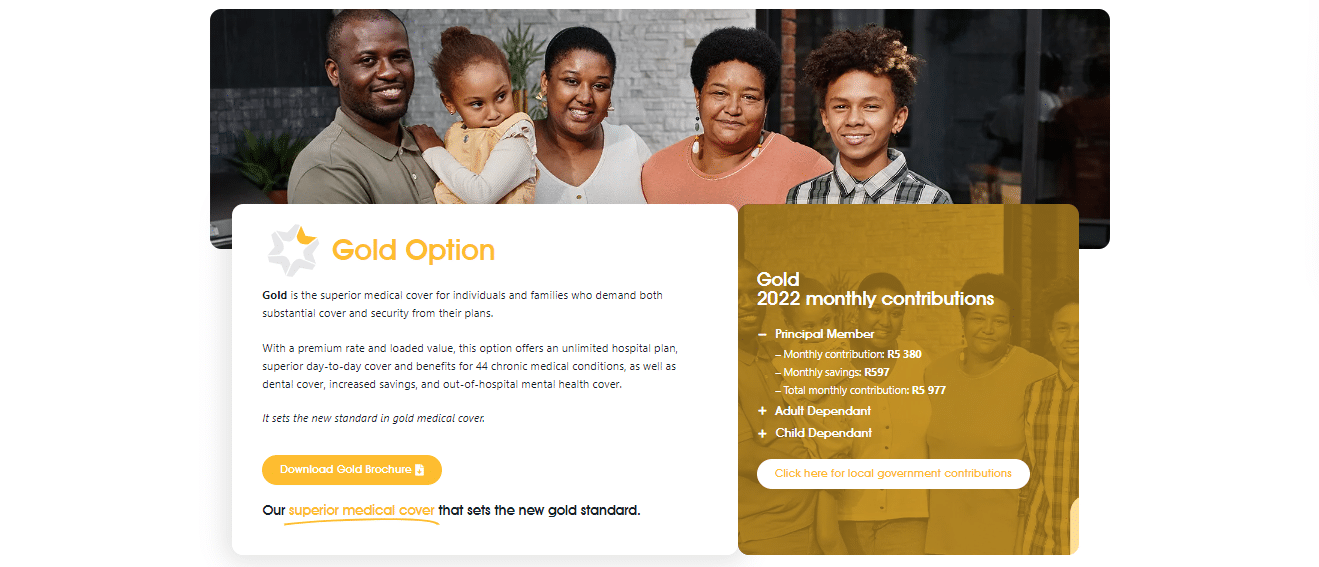
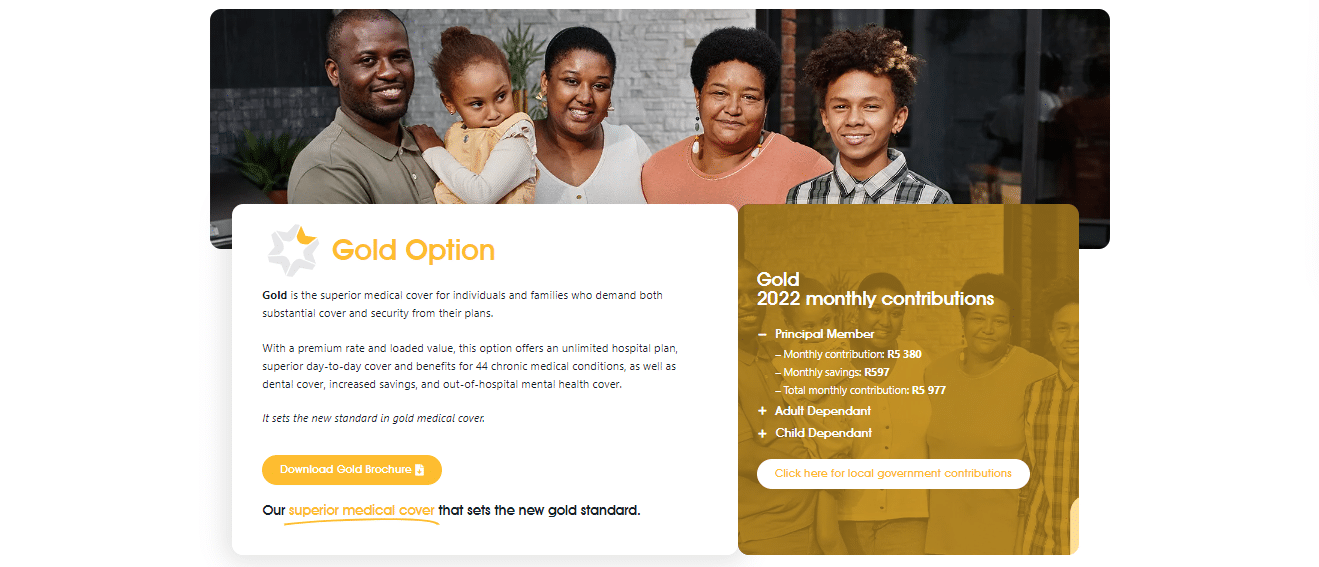
Gold
Gold is the finest medical plan for people and families requiring extensive coverage and security. The Gold option includes an unlimited hospital plan, enhanced day-to-day cover, and benefits for 44 chronic medical conditions, dental cover, increased savings, and out-of-hospital mental health coverage for a premium rate and loaded value.
Hospital Expenses
- All treatment-related expenses at Life Healthcare and Netcare hospitals nationwide, Mediclinic hospitals in the Western Cape, Bloemfontein, Polokwane, and other chosen hospitals (DSP hospital network) will be covered in full.
- Furthermore, there is no limit to the number of hospital admissions. However, all in-hospital operations must be pre-authorized before admission.
- Members get unlimited coverage in-hospital. However, a 30% co-payment will be applied to the hospital bill if a non-DSP hospital is utilized voluntarily.
Injuries resulting from accidents
- Unlimited cover.
- Most incidents are considered PMBs (Prescribed Minimum Benefits), and the scheme will cover the treatment of such injuries, including hospitalization, in full by the Scheme according to its regulations and clinical guidelines.
In-Hospital Specialist Services
- The Scheme covers services rendered by any Specialist while the member is hospitalized.
Oncology
- The diagnosis and treatment of problems associated with cancer.
- The benefit value is up to 461,500 ZAR per family per year.
Scans
- Includes diagnostic scans performed both in and out of the hospital.
- The Benefit Value is R20,000 per family annually for both in-hospital and out-of-hospital benefits. Co-payment of R1 500 for each scan, in or out of the hospital (except for confirmed PMBs).
Sub-acute Facilities and Wound Care
- Covers both in-hospital and out-of-hospital services delivered following an operation or procedure at a rehabilitation or step-down facility and private nursing care to aid in the patient’s recovery.
- Care for wounds is included in this benefit. Benefits value: R46,400 This benefit includes wound care up to an annual maximum of R15,200 per family. Combined in-hospital and out-of-hospital coverage.
Day-to-Day Medical Expenses
- Medical Savings Account (MSA) – A member’s monthly contribution percentage is assigned in advance at the start of the year to an MSA, which is used to pay for routine medical expenses. The MSA can also be used to pay for expenses not covered by the Scheme (such as co-payments, exclusions, etc.) and is carried over to the next year if there is a positive balance at the end of the year. This is a family benefit, which allows one family member to utilize the whole benefit allocation.
- Routine Medical Expenses – Includes general practitioner and specialist consultations, X-rays, prescribed (acute) and over-the-counter drugs, blood tests, physiotherapy, optical, dentistry, etc.
Dentistry
- The plan provides conservative dental care to members, including dentist consultation, x-rays, oral hygiene care, fillings, and extractions.
- Specialized Dental Treatment – Orthodontics (non-cosmetic therapy only). Furthermore, each calendar year, one beneficiary per family can begin therapy. In addition, beneficiaries eligible for treatment are between the ages of 9 and 18.
- The Benefit Value is 80%, subject to scheme conditions.
Chronic Medication
- There is unlimited coverage on the medication used constantly for at least three months to treat one of the 26 CDL (Chronic Disease List) diseases.
- Additional Chronic Medication – Medication used continuously for at least three months to treat 18 chronic illnesses, not on the Chronic Disease List. Each family receives a benefit value of R9,800 per year.
Supplementary Services
- Psychiatric Treatment is an in-hospital benefit that requires pre-authorization. The benefit is 46,400 ZAR per family per year, and case management will apply. Furthermore, for treatment Out-of-Hospital, there is 19,000 ZAR available.
- Prosthesis / Prosthetics / Fixation Devices – 53,800 ZAR is dedicated per family year, a combined benefit. Pre-authorization is compulsory.
- Emergency transport by ambulance – Netcare 911 (provider of DSP) provides members with emergency transport by road or air ambulance from the scene of an accident, as well as medically justifiable inter-hospital transfers.
- Medical Appliances – The provision of medical equipment, such as wheelchairs, crutches, and contraceptive devices, for treating and curing medical disorders or processes. This benefit is 10,300 ZAR per family and year.
- Hearing Aids – The provision of a hearing aid device and its maintenance. Furthermore, the Benefit value is R18 350 per family every five years, with a cap of R9 200 per ear. In addition, on this option, hearing aid servicing (including batteries) is R1,115 per annual beneficiary.
- Endoscopic procedures / Scopes – All scopes are fully covered if performed in a DSP hospital.
Prescribed Minimum Benefits (PMB)
Prescribed Certain Benefits (PMBs) are a set of statutorily defined benefits designed to ensure that all medical plan members are entitled to a minimum level of health care, regardless of the benefit option they have selected.
Additional Benefits
- Easy-ER – Easy-ER is a first-of-its-kind KeyHealth project that provides all KeyHealth members with immediate access to the emergency room (ER) of a hospital for emergency medical care.
- Health Booster – Preventative health care and diagnostic screenings are provided to Scheme participants at no additional cost. However, the Essence option is excluded from this benefit.
- Smart Baby – The Smart Baby Program from KeyHealth provides excellent maternity benefits, support, and general wellness counseling for the pregnant mother.
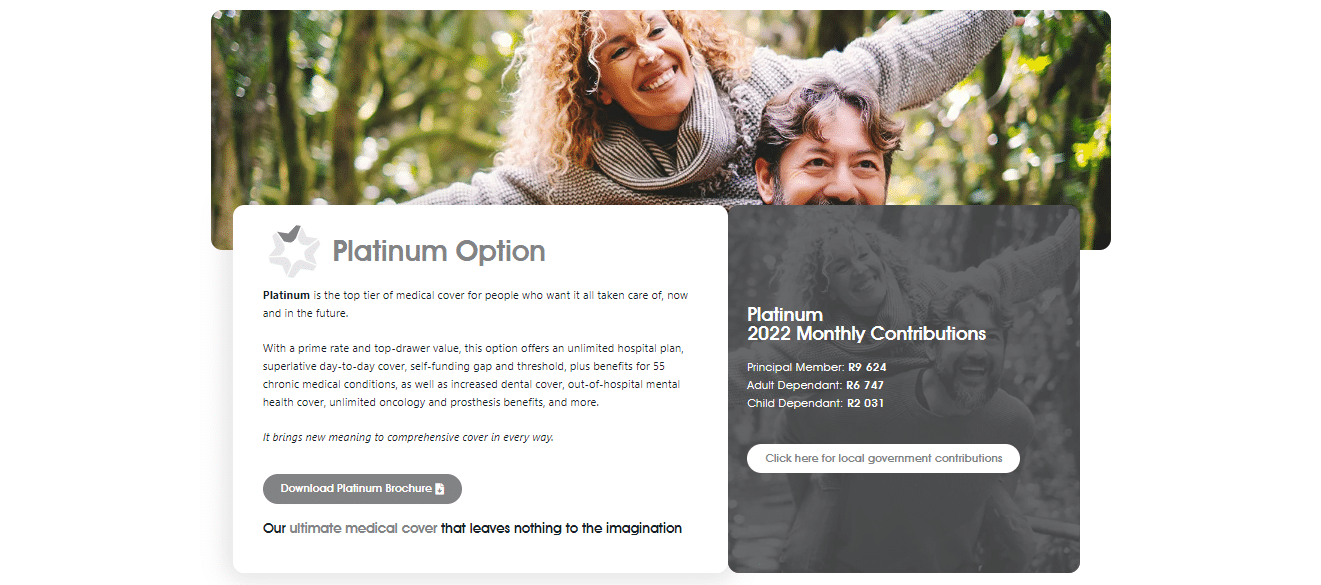
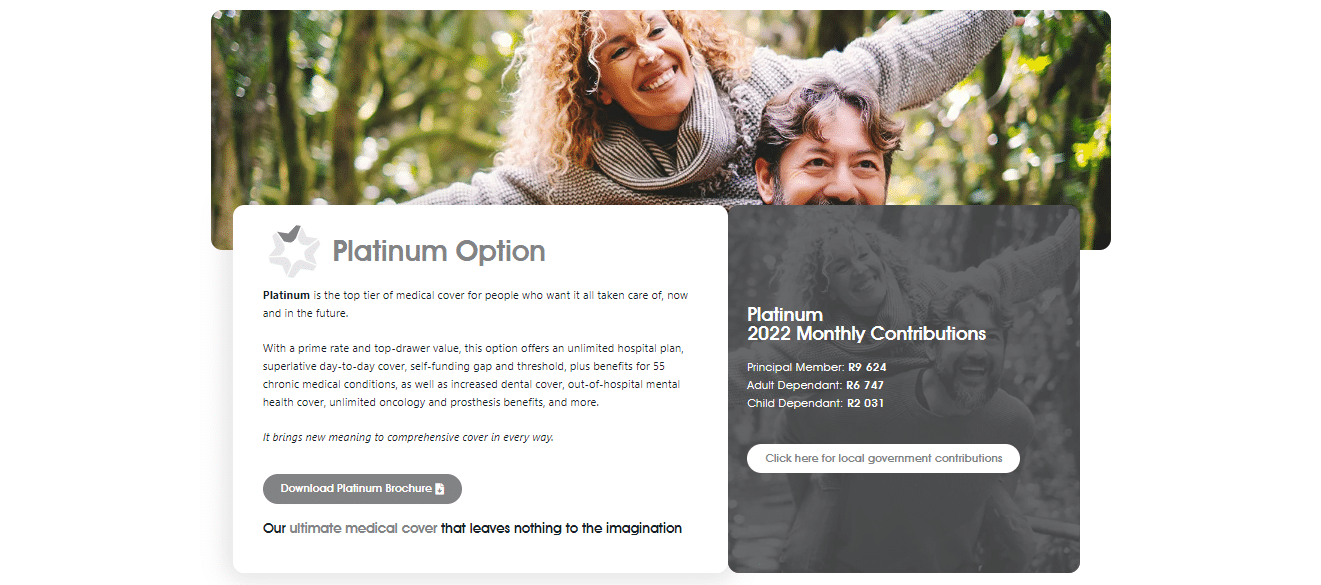
Platinum
Platinum is the highest level of medical coverage for those who want everything taken care of immediately and in the future. The Platinum option offers an unlimited hospital plan, superior day-to-day cover, and a self-funding gap and threshold. Furthermore, the Platinum option offers benefits for 55 chronic medical diseases, expanded dental cover, out-of-hospital mental health cover, and unlimited cancer and prosthesis benefits, all at a premium rate and exceptional value.
Hospital Expenses
- All treatment-related expenses at Life Healthcare and Netcare hospitals nationwide, Mediclinic hospitals in the Western Cape, Bloemfontein, Polokwane, and other chosen hospitals (DSP hospital network) will be covered in full.
- Furthermore, there is no limit to the number of hospital admissions. However, all in-hospital operations must be pre-authorized before admission.
- Members get unlimited coverage in-hospital. However, a 30% co-payment will be applied to the hospital bill if a non-DSP hospital is utilized voluntarily.
Injuries resulting from accidents
- Unlimited cover.
- Most incidents are considered PMBs (Prescribed Minimum Benefits), and the scheme will cover the treatment of such injuries, including hospitalization, in full by the Scheme according to its regulations and clinical guidelines.
In-Hospital Specialist Services
- The Scheme covers services rendered by any Specialist while the member is hospitalized.
Oncology
- The diagnosis and treatment of problems associated with cancer.
- There is an unlimited benefit value of oncology.
Scans
- Includes diagnostic scans performed both in and out of the hospital.
- Benefits value: R28,400 per family annually for both in-hospital and out-of-hospital benefits.
Sub-acute Facilities and Wound Care
- Covers both in-hospital and out-of-hospital services delivered following an operation or procedure at a rehabilitation or step-down facility and private nursing care to aid in the patient’s recovery.
- Care for wounds is included in this benefit. Benefits value: R57,000 This benefit includes wound care up to an annual maximum of R19,700 per family. Combined in-hospital and out-of-hospital coverage.
Dialysis
- The therapy services provided for renal failure.
- There is an unlimited benefit value.
Organ Transplants
- Transplantation of an organ from a donor to a recipient, including administering immunosuppressant medications to avoid organ rejection.
- The benefit value is unlimited on the Platinum option.
Day-to-Day Medical Expenses
- Routine Medical Expenses – Includes general practitioner and specialist consultations, X-rays, prescribed (acute) and over-the-counter drugs, blood tests, physiotherapy, optical, dentistry, etc.
Dentistry
- The plan provides conservative dental care to members, including dentist consultation, x-rays, oral hygiene care, fillings, and extractions.
- Specialized Dental Treatment – Members receive specialized dental care, including crowns and bridges, partial metal dentures, orthodontics, and periodontics.
- The Benefit Value is 80%, subject to scheme conditions.
Chronic Medication
- There is unlimited coverage on the medication used constantly for at least three months to treat one of the 26 CDL (Chronic Disease List) diseases.
- Additional Chronic Medication – Medication used continuously for at least three months to treat 29 chronic illnesses not included on the Chronic Disease List (CDL). The annual benefit value per beneficiary is R21,800, with a maximum of R44,600 per family per year.
Supplementary Services
- Psychiatric Treatment is an in-hospital benefit that requires pre-authorization. The benefit is 64,100 ZAR per family, and case management will apply per year. Furthermore, for treatment Out-of-Hospital, there is a benefit value of 26,700 ZAR.
- Prosthesis / Prosthetics / Fixation Devices – Unlimited funds are dedicated per family year, a combined benefit. Pre-authorization is compulsory.
- Emergency transport by ambulance – Netcare 911 (provider of DSP) provides members with emergency transport by road or air ambulance from the scene of an accident, as well as medically justifiable inter-hospital transfers.
- Medical Appliances – The provision of medical equipment, such as wheelchairs, crutches, and contraceptive devices, for treating and curing medical disorders or processes. This benefit is 13,250 ZAR per family and year.
- Hearing Aids – The provision of a hearing aid device and its maintenance.
Prescribed Minimum Benefits (PMB)
Prescribed Certain Benefits (PMBs) are a set of statutorily defined benefits designed to ensure that all medical plan members are entitled to a minimum level of health care, regardless of the benefit option they have selected.
Additional Benefits
- Easy-ER – Easy-ER is a first-of-its-kind KeyHealth project that provides all KeyHealth members with immediate access to the emergency room (ER) of a hospital for emergency medical care.
- Health Booster – Preventative health care and diagnostic screenings are provided to Scheme participants at no additional cost. However, the Essence option is excluded from this benefit.
- Smart Baby – The Smart Baby Program from KeyHealth provides excellent maternity benefits, support, and general wellness counseling for the pregnant mother.
KeyHealth – Advantages over Competitors
- ☑️ Access to a network of healthcare providers and facilities
- ☑️ Coverage for medical expenses such as doctor visits, hospital stays, and prescription drugs
- ☑️ Financial protection against the high cost of medical care
- ☑️ Choice of coverage levels and options to meet individual needs and budget

KeyHealth Medical Savings Account
KeyHealth offers two plans with a Medical Savings Account: Equilibrium and Gold.
Equilibrium
At the start of the year, a portion of a member’s monthly payment is assigned in advance to an MSA, which is used to cover day-to-day medical expenses. The MSA can also be used to pay for expenses not covered by the Scheme and is carried forward to the next year if there is a positive balance at the end of that year. Because this is a family benefit, only one family member can use the entire benefit allocation.
The benefit value is as follows:
- Main Member – 2,424 ZAR per year
- Adult Dependent – 1,500 ZAR per year
- Child Dependent – 744 ZAR per year
Gold
Medical Savings Account (MSA) – A member’s monthly contribution percentage is assigned in advance at the start of the year to an MSA, which is used to pay for routine medical expenses. The MSA can also be used to pay for expenses not covered by the Scheme (such as co-payments, exclusions, etc.) and is carried over to the next year if there is a positive balance at the end of the year.
This is a family benefit, which allows one family member to utilize the whole benefit allocation. The Benefit value is as follows:
- Main Member – 8,436 ZAR
- Adult Dependent – 5,700 ZAR
- Child Dependent – 1,656 ZAR
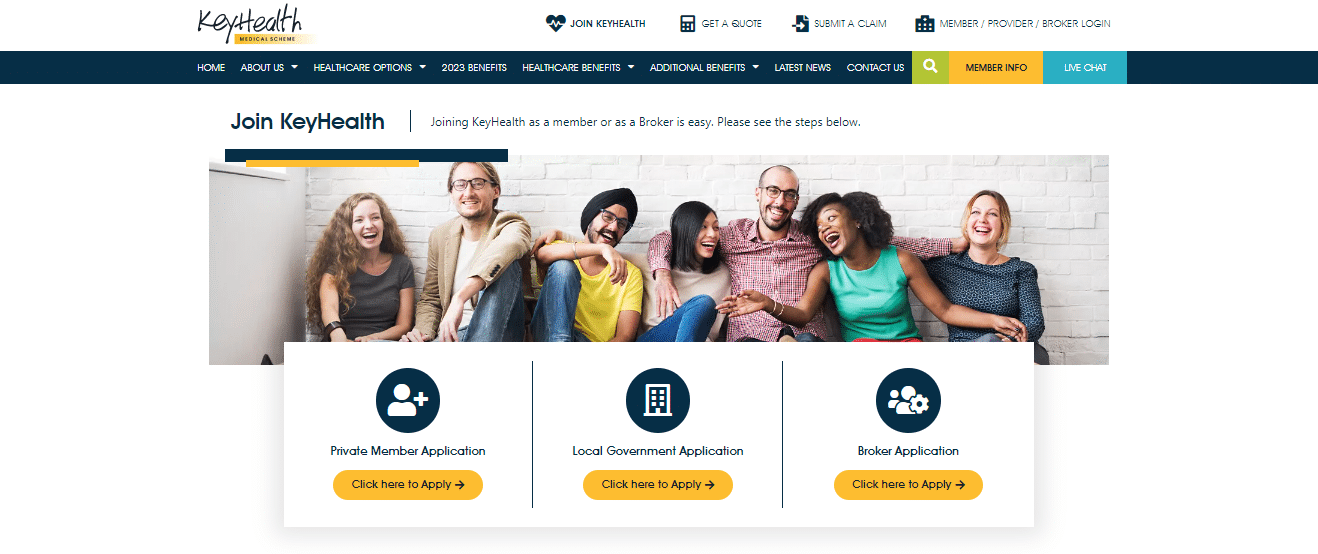
How to apply for Medical Aid with KeyHealth
Medical Aid Quote Keyhealth Medical Scheme process explained
To apply for Medical Aid through KeyHealth, you must:
- Research and compare KeyHealth’s plans: Research the various medical aid plans offered by Keyhealth to determine which one best fits your needs and budget.
- Contact Keyhealth: Once you have decided on a plan, you can contact Keyhealth directly or use an online comparison website to receive a quote.
- Review the plan details: Carefully review the plan details and make sure you understand the terms, conditions, and coverage options included in the plan.
- Complete the application form: Complete the application form provided by Keyhealth, which will typically include personal and financial information.
- Submit the required documentation: Submit the required documentation, such as proof of identity, medical history, and payment information.
- Wait for approval: Wait for Keyhealth to review and approve your application.
- Make the payment: If your application is approved, pay for the first month’s premium.
- Receive your policy documents: After payment is received, you will receive your policy documents, which outline the terms, conditions, and coverage options of your Keyhealth medical aid plan.
- Also take note if you are 35 or older and have not been a member or dependent of a recognized medical scheme continuously since 1 April 2001, without a break in cover exceeding 90 days since that date, you could be subject to a premium loading (late joiner penalty).
Get a KeyHealth Medical Aid quote from our Dedicated Medical Aid Specialists Broker
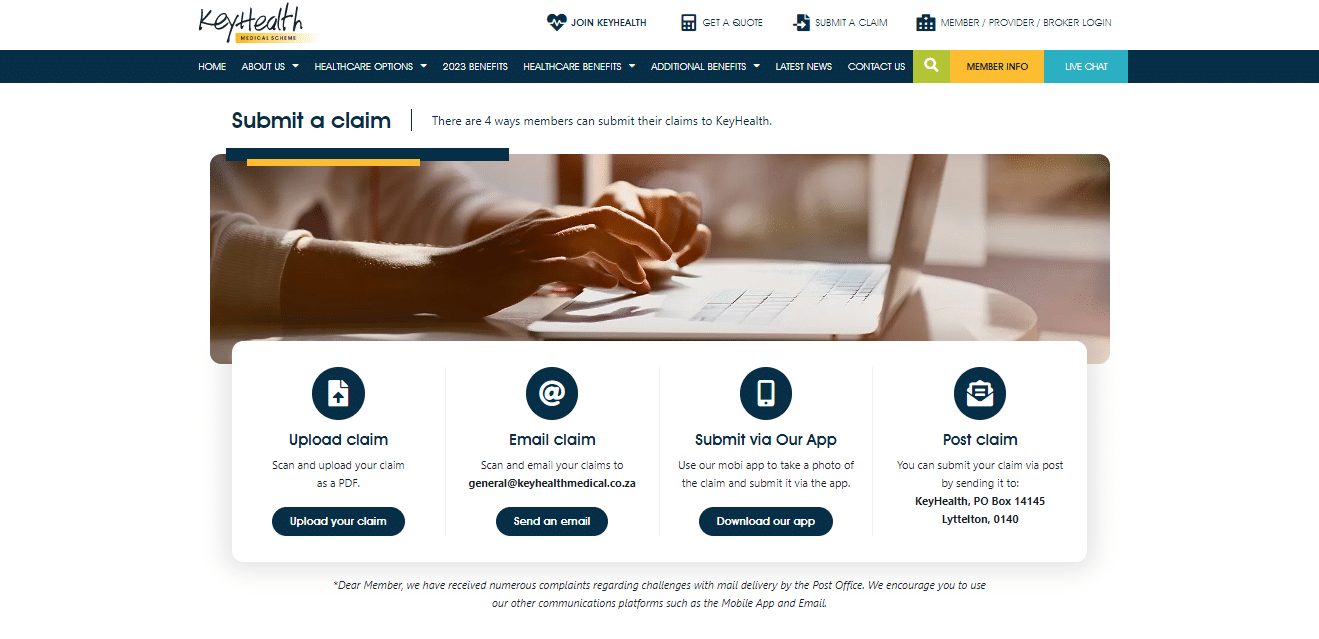
How to Submit a Claim with KeyHealth
To submit a claim to KeyHealth, members can use the following channels:
- Upload the claim in PDF on the website.
- Email the claim to the KeyHealth claims department.
- Submit the claim via the app.
- Post the claim to KeyHealth’s postal address.
How to Submit a Compliment or Complaint with KeyHealth
All complaints against the following must be submitted in writing to the Principal Officer within a reasonable time once the member becomes aware of a problem:
- A KeyHealth member
- A prospective member
- A former member
- A person claiming a benefit by virtue of such a member
- The Scheme or an officer of the Scheme
Furthermore, the complaint should be directed to [email protected].
How to Switch my Medical Aid to KeyHealth
Research the various medical aid plans offered by KeyHealth to determine which one best fits your needs and budget. Once you have decided on a plan, you can contact KeyHealth directly or use an online comparison website to receive a quote. Carefully review the details of the plan, including the terms, conditions, and coverage options, to make sure it meets your needs. Provide KeyHealth with proof of your current medical aid coverage, such as a copy of your current medical aid card or a letter from your current medical aid provider. Complete the application form provided by KeyHealth, which will typically include personal and financial information. Submit any required documentation, such as proof of identity and medical history. Wait for KeyHealth to review and approve your application.
Also take note that New Members 35 years or older may be subject to late-joiner penalties on KeyHealth Medical Aid Plans.
KeyHealth vs Discovery Health vs Bonitas – A Comparison
| 🔎 Medical Aid | 🥇 KeyHealth | 🥈 Discovery Health | 🥉 Bonitas Medical Fund |
| 📌 Years in Operation | – | 30 Years | 40 Years |
| 📍 Average # Members | 150,000 | 3.3 million | 750,000+ |
| 📈 GCR Rating | – | AAA | AA |
| 📉 Number of Employees | 500+ | 13,500 | 150+ |
| 📊 Market Share | | 56.7% | +-25% |
| ➡️ Market Cover | South Africa | 40 Markets | South Africa |
| ❤️ Customer Rating | 3/5 | 4.4/5 | 4.9/5 |
| ✔️ Number of reviews | 200+ | 20,000+ | 5,000+ |
| 📱 Mobile App | ✅ Yes | ✅ Yes | ✅ Yes |
| 💵 Contribution Range (ZAR) | 1,990 – 11,308 ZAR | 1,102 – 10,303 ZAR | 1,378 – 9,853 ZAR |
| 💶 International Travel Benefit (ZAR) | Between 2.5 and 6 million ZAR per beneficiary | Up to 5 million ZAR | Up to 10 million ZAR |
| 💳 Market Capitalization | – | 86.2 billion ZAR | – |
Compare KeyHealth plans with other medical aid providers:
- 📌 KeyHealth vs Discovery Health
- 📌 KeyHealth vs. Bonitas
- 📌 KeyHealth vs. BestMed Medical Scheme
- 📌 KeyHealth vs. Fedhealth
- 📌 KeyHealth vs. Medihelp
- 📌 KeyHealth vs. Medshield
- 📌 KeyHealth vs. Momentum Medical Scheme
- 📌 KeyHealth vs. Sizwe Hosmed Medical Fund
KeyHealth Member Reviews
Great Outcome.
Initially, Key Health declined to pay any expenses related to the hospital stay at Hilton Life. However, after consultations with specialists and the hospital’s case managers, they agreed to cover all aspects of the stay. – Bella Garrison

Excellent.
I would like to extend my sincerest gratitude to Key Health for their professionalism and efficiency during difficult times. The passing of my father-in-law after 66 years of marriage was a devastating event for my mother-in-law. Key Health demonstrated respect and understanding, ensuring she was fully covered as the principal member. I commend the entire team at Key Health for their support during this challenging period. – Maddison Lucas

Happy Member.
I recently discovered that the tax submissions for my mother-in-law had not been completed since the passing of my late father-in-law. So, I requested tax certificates for the period from 2013 onwards and was pleasantly surprised to receive them via email within hours. This commitment to excellent service is highly commendable, and I am proud to have been on the receiving end of it. – Jane Grant

KeyHealth – Our Verdict
KeyHealth Medical Aid is a South African medical aid scheme that provides access to healthcare services for its members. Advantages of KeyHealth Medical Aid include a range of comprehensive medical aid options, competitive pricing, and access to a network of healthcare providers. Furthermore, medical aid offers a range of benefits, including cover for in-hospital treatment, chronic medication, and maternity benefits. Drawbacks of KeyHealth Medical Aid include limited access to certain medical specialists and limited options for hospital cover. Additionally, members could be required to pay co-payments or have a waiting period for certain medical services.
KeyHealth Pros and Cons
| ✅ Pros | ❎ Cons |
| KeyHealth is focused on providing comprehensive hospital coverage with some additional benefits | There are only a few chronic conditions covered |
| There are six flexible plans to choose from | KeyHealth is not as flexible as most competitors in South Africa |
| There are additional benefits offered for each plan | There are several services that members must pay for themselves |
| The plans are affordable when compared to other medical aids | There is no native gap cover provided |
KeyHealth Frequently Asked Questions
What is Keyhealth?
Keyhealth is a medical aid scheme and insurance provider in South Africa. They offer a range of healthcare plans to individuals and families at affordable prices. Keyhealth covers a variety of medical services, including hospitalization, chronic medication, specialist consultations, and day-to-day benefits like dental and optometry coverage. They have a designated service provider (DSP) network that includes healthcare providers who have agreed to charge lower rates for Keyhealth members. Keyhealth is known for its comprehensive hospital plans and affordability, making it a popular choice for many South Africans.
Is Keyhealth a part of Discovery Medical Aid?
Keyhealth is an independent medical aid fund in South Africa. It should not be confused with the Keycare option provided by Discovery.
How much is KeyHealth Medical aid per month?
KeyHealth’s plans start from 1,990 ZAR on the Essence option to 11,308 ZAR on the Platinum option.
Where can I find the KeyHealth portal?
You can visit the KeyHealth website to find the login portal on the homepage.
Is KeyHealth medical scheme a good option?
KeyHealth is a good option for those seeking a comprehensive and all-inclusive hospital plan.
What are the KeyHealth medical scheme contact details?
KeyHealth can be contacted telephonically at 0860 671 050 and via email at [email protected].
Where can I view the KeyHealth medical aid prices?
You can view the KeyHealth medical aid prices on the official website under Healthcare Options.
What primary care services are covered by KeyHealth?
KeyHealth covers a range of primary care services, including GP consultations, medication, and diagnostic tests.
Does KeyHealth cover specialist consultations?
Yes, KeyHealth covers specialist consultations, including specialist fees, diagnostic tests, and procedures.
Does KeyHealth cover prescription medication?
Yes, KeyHealth covers the cost of prescription medication, subject to certain limitations and restrictions.
Is KeyHealth affordable?
Yes, KeyHealth is an affordable medical aid option with various plans and options to suit different budgets.
Can families be covered under KeyHealth?
Yes, KeyHealth offers a range of family plans, which can cover up to four children under 21.
Does KeyHealth offer dental coverage?
Yes, KeyHealth offers dental coverage as part of its day-to-day benefit, which covers routine dental procedures.
Does KeyHealth offer optometry coverage?
Yes, KeyHealth offers optometry coverage as part of its day-to-day benefit, which covers routine eye tests and prescription glasses.
How do I reset my KeyHealth login?
You can click the “Forgotten your login or password” link on the login page to reset it.
How do I Downgrade my Plan with KeyHealth?
Review your current KeyHealth plan to determine which coverage options you no longer need and Contact KeyHealth directly to request a downgrade of your plan.
How do I add a Beneficiary to KeyHealth?
If you want to add a child or adult dependent, you can log into your KeyHealth profile and download and complete the “Application to Register a Dependent,”
How do I access my KeyHealth login?
You can access your KeyHealth login by visiting the KeyHealth website and logging in using your username and password.
What is KeyHealth DSP?
KeyHealth DSP is a designated service provider network that includes a range of healthcare providers who have agreed to charge lower rates for KeyHealth members.
What are KeyHealth waiting periods?
KeyHealth waiting periods are when new members must wait before claiming certain benefits under their medical insurance policy.
How do I access my KeyHealth login?
You can access your KeyHealth login by visiting the KeyHealth website and logging in using your username and password.
What services are covered by KeyHealth?
KeyHealth covers a range of services, including hospitalization, chronic medication, maternity care, and specialist consultations.
How do I join KeyHealth?
You can join KeyHealth by visiting their website, filling in the online application form, and submitting the required documents.
How do I choose the right KeyHealth plan for me?
KeyHealth offers a range of plans to choose from. Consider your budget, health needs, and the level of coverage you require before selecting a plan.
Can I add my family members to my KeyHealth plan?
Yes, you can add your spouse and children to your KeyHealth plan.
How do I submit a claim to KeyHealth?
You can submit a claim to KeyHealth by completing the relevant claim form and providing the required supporting documents. Claims can be submitted via email, fax, or post.
How long does it take for KeyHealth to process claims?
KeyHealth aims to process claims within 5 working days.
How do I find a KeyHealth-approved healthcare provider?
You can find a list of KeyHealth-approved healthcare providers on their website or by calling their customer care center.
Does KeyHealth cover pre-existing conditions?
Yes, KeyHealth covers pre-existing conditions after a waiting period has been served.
How do I change my KeyHealth plan?
You can change your KeyHealth plan by contacting their customer care center or completing the online plan change form.
What happens if I miss a premium payment?
Your cover may be suspended or terminated if you miss a premium payment. Contact KeyHealth as soon as possible to arrange to pay your outstanding premiums.
Can I suspend my KeyHealth coverage?
Yes, you can suspend your KeyHealth coverage for 3 months. After that, a suspension fee may apply.
What happens to my KeyHealth cover when I retire?
KeyHealth offers a range of retirement options to its members. Contact KeyHealth to find out more.
What is the KeyHealth mobile app?
The KeyHealth mobile app is a convenient way for members to manage their medical aid coverage, submit claims and find healthcare providers.
Can I access my KeyHealth account online?
Yes, you can access your KeyHealth account online by logging in to their website.
Does KeyHealth offer wellness programs?
Yes, KeyHealth offers a range of wellness programs, including health screenings, nutrition advice, and exercise programs.
How do I cancel my KeyHealth coverage?
You can cancel your KeyHealth coverage by completing the relevant cancellation form and submitting it to KeyHealth.
What is the KeyHealth loyalty program?
The KeyHealth loyalty program rewards members for staying with KeyHealth for 3 years or more.
How do I contact KeyHealth customer care?
You can contact KeyHealth customer care by calling their toll-free number or emailing their customer care center. Contact details can be found on their website.
Are there any reviews available for KeyHealth?
Yes, many reviews are available online for KeyHealth, which can provide valuable insight into the experiences of current and former members.
Does KeyHealth cover chronic conditions?
Yes, KeyHealth covers certain chronic conditions such as HIV/AIDS, diabetes, and hypertension.

Adriaan Schoeman
Adriaan holds an MBA and specializes in medical aid research. With his commitment to perfection, he ensures the accuracy of all data presented on medicalaid.com every three months. When he is not conducting research, Adriaan can be found indulging in his passion for trout fishing amidst nature.